Semantic interoperability – towards realizing the intend of EHR standards
Semantic interoperability of EHR data is the foundation for advancing healthcare because, in today’s value-based market, availability of the required information is critical to making the right decisions. To do what’s best for patients, providers need to share critical information to help coordinate care across the entire continuum.
Every time a person visits a primary care provider (PCP), health information is being added to their own electronic health record (EHR). Where does that information go? The answer, currently, is nowhere, unless it is transcribed into a referral and sent to a specialist. And even then, it’s only partial information that is provided to the specialist – not the entire medical record.
There is no “shared care record.” Information about the individual exists in multiple EHRs, so no one has the complete picture of your health.
In 2004, United States created the Office of the National Coordinator for Health Information Technology (ONC) with the aim of introducing the notion that Health Information Technology (HIT) should be nationally coordinated. One of the first endeavors of ONC was the planning and design of a National Health Information Network (NHIN) as a means to facilitate the exchange of electronic health information among providers and Health Information Exchange (HIE) entities.
However, in spite of the above initiative, EHRs have largely remained siloed in their data repositories and have proven highly inefficient for sharing machine-processable information among providers caring for a patient. The real impact of digital information is yet to reach a level adequate to enrich patient care outcomes or greatly increase surgical decision making. Some EHR systems have been accused of data blocking and adding service costs for providers seeking more effective means of data sharing.
Moving from interoperability to semantic interoperability
When digital systems seamlessly exchange data with each other, it is referred to as interoperability. More specifically, true interoperability occurs when information held in one EHR transfers through a standardized wire format to a separate EHR, in such a way that the information that is exchanged proves to be machine readable by the accepting EHR. Once that information is transferred, the receiving EHR should be capable of understanding the content and the context of the data shared for it to be able to represent the information appropriately in the workflow of the clinicians using the transferred information.
A clinical record can contain more than 100,000 different data fields and elements including numeric data, structured text, unstructured text and scanned files and images. To get these different systems talking to each other – exchanging data – context is critical. Without the correct context, medical professionals can overlook information.
From a usefulness perspective, there are three levels of interoperability:
- Foundational interoperability allows data exchange from one information technology system to be received by another and does not require the ability for the receiving information technology system to interpret the data.
- Structural interoperability is an intermediate level that defines the structure or format of data exchange where there is uniform movement of healthcare data from one system in a way that preserves and does not alter the clinical or operational purpose and meaning of the data.
- Semantic interoperability provides interoperability at the highest level – the ability of two or more systems or devices to exchange information and to use the information that has been exchanged. This level of interoperability supports the electronic exchange of patient summary information among caregivers and other authorized parties via disparate electronic health record (EHR) and other systems.
Interoperability of EHR supports collaboration between providers, which can reduce medical errors, misdiagnoses as well as repetitive, costly diagnostic tests. This is especially true for chronically ill patients who visit multiple physicians and specialists.
From a process improvement perspective, interoperability allows healthcare professionals to access data on specific populations of patients to develop best practices that are proven to improve outcome while controlling costs. When researchers pull clinical as well as financial data to evaluate treatment, outcomes and costs, they are better able to identify strategies to address gaps in care – which benefits patients, payers and healthcare organizations.
Challenges to achieving semantic interoperability
Though the need is understood well land accepted in all academic circles, the field reality is far from this due to many problems.
- Lack of universal standards-based EHR system adoption
- Impact on providers’ workflow.
- Complex privacy and security challenges
Enablers that can improve the situation
- Quality APIs that are based on industry standards
- A cloud-based platform
One may assume that the interoperability efforts of the next several years will be shaped by pursuing the path that has guided the industry for the past several years: defining data standards, advancing the incentives that encourage exchange, ensuring privacy, certifying the interoperability capabilities of EHRs and addressing issues such as data blocking.
Deciding factors
- Govt’s stand on deciding standards and regulatory bodies.
- Adaptation of the medical industry towards changing technology
- Proactive tech industry to building tools for medical industry
In the Electronic Health Record Standards for India, 2016, the government stated that ‘the prime aim of interoperability standards in India is to ensure syntactic (structural) and semantic (inherent meaning) interoperability of data amongst systems at all times’. With this and other related policy initiatives, Indian government has demonstrated it’s commitment towards interoperability of EHR for it’s citizens.
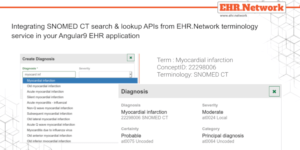
Our EHR.Network platform will help your applications quickly achieve semantic interoperability. We have designed it with developers like you in mind and to make things easy for you.
Resources:
- http://www.mdpnp.org/uploads/1_Robkin_26Jan.pdf
- https://hitconsultant.net/2013/04/11/history-of-healthcare-interoperability/#.XIAmeC-B2u4
- http://bulletin.facs.org/2017/11/a-history-of-health-information-technology-and-the-future-of-interoperability/
- https://www.himss.org/news/current-state-interoperability
- https://www.hhnmag.com/articles/7689-the-evolution-of-interoperability-in-health-care
- https://www.allscripts.com/news-insights/blog/blog/2018/02/interoperability-for-all
Learn more
- Explore case studies
- Read documentation
- Write to us
- Call us on +91 63609 97311








0 Comments